Analysis by a Midwestern Doctor
History at a Glance
- During the COVID-19 pandemic, an estimated one million Americans have died due to poor hospital care and the suppression of effective off-patent therapies. Much of this is because Obamacare has forced hospitals to aggressively treat patients so they can leave the hospital quickly and reduce healthcare costs.
- Frailer patients respond poorly to aggressive protocols, resulting in them often being sent to palliative care or hospice. Unfortunately, doctors are no longer trained to gradually nurse their patients back to health, and so they view many of these deaths as inevitable.
- During the COVID-19 pandemic, hospitals implemented strict protocols that focused on remdesivir and ventilators while refusing alternative treatments, even when patients were likely to die—in one notable example, patients who received court-ordered ivermectin achieved a 95% survival rate, compared to just 5% for patients who were denied.
- Current medical training emphasizes following standardized protocols rather than practicing personalized medicine. Junior doctors are trained to perform procedures rather than critically examine cases and tailor treatment plans for each patient.
In this article, we look at some of the forgotten medical therapies that are dramatically improving hospital outcomes, and highlight some of the key strategies that patients and policymakers can use to reduce hospital deaths.
During COVID-19, we have witnessed something we could not have imagined before. The national emergency sent thousands of Americans to the hospital, cut off from their loved ones and inevitably dying. It quickly became clear that hospital protocols were not working, but no matter how futile conventional care was, patients in our hospitals were unable to receive the alternative therapies they needed.
This led to a sobering realization across America that what many of us had believed about our hospitals was completely wrong. Instead of helping patients, hospitals were effectively operating like assembly lines, implementing disastrous protocols (like remdesivir), denying patients access to their loved ones, and refusing to use alternative therapies even when it was known that patients would otherwise die.
This was best illustrated by a travel nurse who was sent to a New York hospital with the highest death toll in the country and realized that something very wrong was happening throughout the hospital, so she secretly recorded it:
🧵Nurse Erin worked in NYC at the hardest hit COVID hospital in America. She witnessed a horrifying number of needless deaths and exposed why so many people actually died.
This secret recording shows how doctors would not treat patients they knew would die with anything except… pic.twitter.com/GONAsB6QVt
— A Midwestern Doctor (@MidwesternDoc) November 26, 2024
Note: The entire interview provides clear evidence that many patients were killed due to grossly inadequate hospital protocols. You can see a similarly shocking testimony from another NYC COVID nurse on my Twitter account here.
Shockingly, the COVID-19 treatment protocols offered financial incentives for remdesivir (“death is near”) and then ventilation, but disfavored effective, off-patent treatments. So hospital administrators demanded deadly “treatments” like remdesivir and punished doctors who used unprofitable treatments that saved lives.
Note: The NIH continued to promote remdesivir as a treatment for COVID-19 and banned alternative therapies, despite the evidence accumulated in the protocols. This was because Anthony Fauci appointed the NIH committee and selected chairmen who had direct financial ties to the makers of remdesivir—a recurring problem in American medicine (for example, I showed how our grossly inaccurate cholesterol guidelines were written by people who took money from statin manufacturers, here ).
Because of this murderous corruption, families began suing hospitals to allow the use of ivermectin for a loved one who was expected to die (after being subjected to Fauci’s COVID hospital protocols). It is noteworthy that the hospitals chose to fight these lawsuits in court rather than simply administering the ivermectin, because so much money was at stake.
Of the 80 lawsuits filed by attorney Ralph Lorigo, the judge ruled in favor of the family in 40 cases and the hospital in 40 cases. Of the 40 cases where patients received ivermectin, 38 survived, while of the 40 cases where they did not, only 2 survived—making the lawsuit against the hospital arguably the most effective medical intervention in history. But instead of considering this data, for-profit hospitals banded together to develop an effective mechanism to dismiss further lawsuits.
Because I expected this to happen, I implemented simple home treatments (e.g., purchasing high-powered oxygen concentrators and noninvasive ventilation) just before the pandemic. Many people in my immediate community have been successfully treated at home, many of whom would otherwise have been immediately hospitalized and likely died.
Note: Before COVID, we had other patients who deserved hospitalization but who would likely have been admitted to hospice care upon admission. So we have already learned how to provide much of the care we need at home.
Likewise, during the pandemic, I have heard countless stories in which a relative provided “unapproved” therapy to a patient in the hospital, thereby saving the patient’s life.
Reductionist Reality
Every situation has two sides: the material factors and the intangible processes that lie between them. While modern science often focuses on optimizing the tangible, it tends to overlook the deeper nature of each phenomenon. Those who nevertheless master these intangible aspects excel at solving a variety of problems that their colleagues cannot solve.
In medicine, this is clearly seen in the contrast between algorithmic care—in which doctors follow strict protocols—and the art of medicine, which involves critical thinking, individualized treatment plans, and nurturing the doctor-patient relationship that is essential to recovery. The importance is.
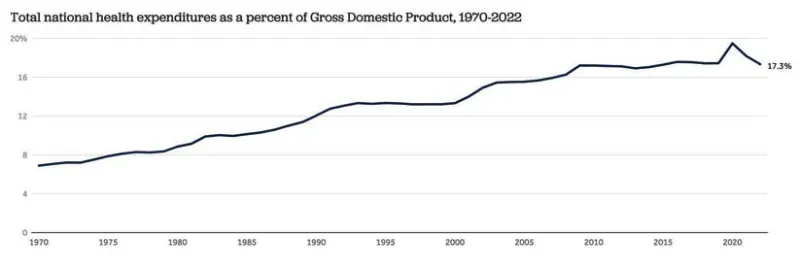
Unfortunately, medical education has increasingly shifted from supporting independent judgment to favoring corporate-driven policies, leaving little room for the art of caring. In parallel with this shift, the cost of American health care has skyrocketed:
Note: Healthcare spending was 0.25% of GDP in the early 20th century.
It is remarkable that despite spending two to four times more on healthcare than any other rich country, the United States has the worst healthcare outcomes among rich countries.
I believe this is because our healthcare spending prioritizes corporate interests over what makes for effective healthcare delivery, and because pervasive corruption is entrenched throughout government.
Economic Incentives
One of the most reliable tools a government has to change the behavior of the healthcare system is to financially support desirable behaviors (e.g., promoting remdesivir).
An important part is evaluating hospitals based on the quality of care they provide to patients and hospital reimbursement rates tied to their “quality.” Unfortunately, while some metrics are useful (e.g., what percentage of patients get infected in the hospital), many other metrics that lobbyists push are not (e.g., what percentage of patients are vaccinated). As a result, hospital administrators often force healthcare professionals to enforce policies that harm patients.
Note: JCAHO is the primary organization that evaluates the quality of care provided by hospitals. Hospital administrators, in turn, go to great lengths to appease JCAHO.
After 40 years, healthcare spending has been increasing exponentially, with 22% of all medical spending (and 26% of Medicare spending) occurring in the last year of life. Since there has always been a risk of Medicare (and Social Security) going bankrupt, reducing these costs has long been a focus of healthcare bureaucrats (as far as I know, it started in 1979, but it really took off with Obamacare).
The high cost of hospital stays—an average of $2,883 per day, or up to $4,181 in California—has made reducing their length a priority for health care administrators.
For example, hospitals receive a flat rate for admission regardless of how long a patient stays (resulting in the hospital having to cover the cost of longer stays), and critical care hospitals (which receive more money) must keep average lengths of stay below 96 hours to maintain JCAHO and Medicare accreditation.
As a result, hospitals often pressure physicians to reduce lengths of stay through financial rewards or penalties for “excessive” stays, with boards aggressively reviewing and challenging any extended admissions.
Note: Emergency room physicians’ decisions about whether to admit patients to the hospital also vary widely. Some are more cautious, admitting patients who may not be that sick to avoid liability, while others are selective, admitting only patients with clear serious illnesses. This unnecessary revenue strains hospital resources and causes insurance companies to have unrealistic expectations about how quickly many illnesses will improve and patients will be able to leave the hospital.
Time to heal
Whenever there is a problem in medicine, the bureaucratic tendency is to look for ways to manage tangible variables at the expense of intangible aspects of patient care. As a result, almost all protocols in which doctors are trained (“improvement of the quality of medical care”) tend to push intangible aspects aside—to the point that doctors are often penalized for deviating from protocols.
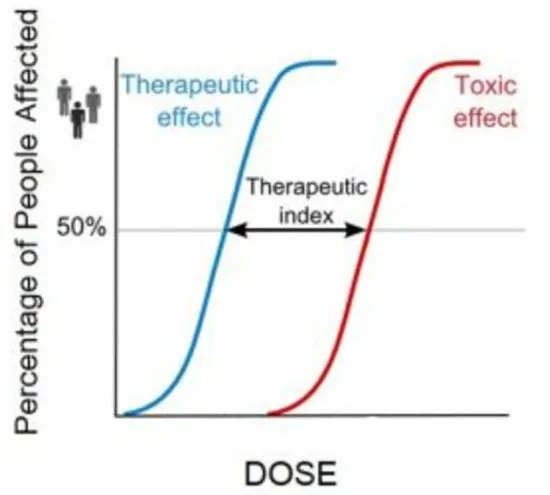
One area where this is particularly problematic is dosing, since different patients simply require different doses of the same therapy. For almost all therapies, there is a certain dose at which most patients benefit from the therapy and another at which they experience toxicity.
Dosage is usually determined based on the average of these two values (the therapeutic index). The problem is that patients’ sensitivity to treatments varies so much that a therapeutic dose for one patient may be toxic to another. Since a standardized medical system cannot function without standardized doses, doses are used that often harm the more sensitive members of the population.
Note: The art of dosage and the methods we use to determine the correct dose for patients are explained in more detail here.
For example, it is recognized in almost every naturopathic practice that “frail” patients usually cannot tolerate higher doses and that their treatment requires lower doses for a longer period of time. However, because hospitals are “forced” to discharge patients quickly, higher doses are usually given, allowing patients with more robust constitutions to recover quickly, but the frail patients are overrepresented.
Unfortunately, in such cases, family members are often told, “There is nothing more that can be done for the patient” or “He would not want to live like this for the rest of his life,” in order to pressure them to bring their relatives into the family, provide palliative care so that he can die “with dignity,” or send him to hospice.
We believe that this inappropriate dosing is a major cause of unnecessary deaths in hospitals, and that many “incurable” cases could recover with slower treatment.
For example, patients with congestive heart failure are usually given aggressive diuretics to remove excess fluid from the body. In more robust patients, this works and they can be discharged within 2 to 3 days, but in weaker patients, it can cause a number of serious complications (e.g., hyponatremia or kidney failure). In these patients, good results can be achieved with only 4 to 5 days of hospitalization and a gentle, well-balanced diuretic protocol.
Note: A similar problem occurred during the COVID pandemic when patients were prematurely removed from ventilators.
Because of these economic incentives, hospitals have become very efficient at steering patients through palliative care, and hospital care often becomes a Darwinian situation where you are “selected” to die if you don’t recover within 3 to 4 days.
In short, hospitals are encouraged to “treat” patients with a standardized protocol rather than nurse them back to health. As a result, many of the actions needed to improve patient outcomes are not taken, and critical resources are inappropriately diverted.
For example, hospitals routinely invest in social workers to expedite patient discharge (e.g., by pushing). In contrast, hospitals are so understaffed that nurses often only have time to take vital signs and administer prescribed medications, rather than checking in with each patient every few hours, let alone checking in on how they are doing (which is often crucial to a patient’s recovery).
Ideally, nurses should be assessing patients every 2 to 3 hours. Spending a little more money on 1 to 2 more nurses on each floor would be a relatively inexpensive way to dramatically improve patient outcomes.
Ultimately, we believe that the push to quickly discharge patients from hospitals (e.g., nursing homes), rather than saving money, actually increases healthcare costs because early discharges often lead to high readmissions—which is especially tragic because multiple hospitalizations often drag patients into a fatal downward spiral.
Note: In contrast, accelerated hospitalizations are far less problematic for postoperative patients because surgeons are financially penalized if their patients die within 30 days of surgery, and therefore have an incentive to keep patients in the hospital long enough. This shows that many things in medicine are based on economic incentives rather than what is best for the patient.
Training Priorities
This new paradigm is largely due to junior doctors being trained to follow protocols and request consultations, rather than critically examining each case, identifying what they are missing, and trying to tailor their treatment plan to each patient (e.g., the past was much more about adjusting dosages).
Most notably, doctors are being trained to accept the inevitability of many illnesses that are actually completely treatable (with the right approach).
To illustrate, I recently had a colleague whose father was discharged to a hospice center and started palliative care because his case was terminal. However, my colleague was (correctly) convinced that he was just dehydrated and needed saline. Four days later, they called me in tears and I said, “Well, you’re a doctor, can’t you get them to give him an IV?” , so I need help.
Unfortunately, many doctors don’t even know they are failing their patients because current training is based on the assumption that hospital stays should last three to four days, and they never lived in a time before these regulations where it was possible to recognize the benefits of longer hospital stays.
Therefore, we need to shift our focus from optimizing the palliative pathway and financial incentives for patient survival rather than length of stay, because without these incentives, doctors are not trained to save lives, nor do they have the autonomy to do so in the best interests of their patients.
Note: Preventing readmission to hospital (especially for patients in a downward spiral) often requires effective integrative medical care outside the hospital (another area in which current medical education does not educate doctors).
Life-Saving Measures
At the turn of the 19th and 20th centuries, conventional medicine was on the verge of extinction because natural therapies were much safer and more effective. To “save” medicine, the American Medical Association (AMA) teamed up with industry and the media to monopolize healthcare and eliminate all competition by branding it quackery. As a result, between the 1920s and the 1960s, many remarkable therapies (which I regularly use in my practice) were blacklisted and forgotten.
Many of these treatments initially became famous for the miraculous results they produced on terminally ill patients in the hospital.
For example, ultraviolet blood irradiation (UVBI) was remarkably effective for a variety of infections where antibiotics had failed (or did not work, such as viral pneumonia), and doctors soon discovered that it could also be used for autoimmune diseases (e.g., asthma exacerbations), circulatory disorders (e.g., heart attacks), and surgical procedures (e.g., to prevent infections, restore bowel function, and speed healing).
Unfortunately, after taking our hospitals by storm, it was blacklisted by the AMA (resulting in the relocation of UVBI to Russia and Germany) and despite hundreds of studies demonstrating its immense value (discussed here), it remains blacklisted by our medical system. .
Note: UVBI is widely used in integrative medicine (because it safely treats many different serious medical conditions) and is one of the primary therapies I use.
Likewise, sepsis (which still kills 350,000 Americans each year despite our “best” efforts) responds remarkably well to early intravenous vitamin C. Paul Marík, for example, was able to use it to reduce sepsis mortality in his hospital from 22% to 6% (and in one study showed that mortality dropped from 40.4% to 8.5%).
Similarly, in the (rare) hospitals we have worked in that use intravenous vitamin C, sepsis deaths are extremely rare. Yet this approach is demonized and nearly impossible to obtain for a loved one in the hospital.
I have also recently begun to highlight another remarkable, forgotten therapy, DMSO (e.g., it is arguably the safest and most effective pain treatment available—which in turn has led to hundreds of readers reporting that DMSO has given them their lives back).
DMSO is also effective in treating heart attacks, strokes, brain hemorrhages, traumatic brain injuries, and severe spinal cord injuries (areas where medicine can do little), and there is evidence that DMSO, if used in our hospitals, would save millions of lives, potentially saving people from living with disabilities or paralysis.
Note: There are many other ways to optimize hospital care. For example, we found that intravenous amino acids significantly increase the speed and likelihood of recovery, but they are only available in hospital formulations (TPN) that also contain toxic seed oils and are more likely to make patients sick than to cure them. Similarly, we were able to save seriously ill COVID patients during the pandemic through neglected, off-patent therapies.
Conclusion
COVID-19 has shattered the unconditional trust that the medical industry has invested and relied on tremendously for decades (e.g., a large JAMA study of 443,445 Americans found that 71.5% of them trusted doctors and hospitals in April 2020, compared to just 40.1% in January 2024).
A question I’ve gotten from many insiders since the election is, “What do we need to do to increase survival rates in our hospitals? I believe that is a critical key to making America healthy again.” If clinical trials were conducted on the approaches described in this article (which the medical industrial complex has predictably always blocked), they would show immediate and undeniable benefits in terms of mortality.
I sincerely hope that our unique political climate will open a window for testing these forgotten approaches in hospital care, especially as their validation in the acute setting creates an openness for their application to chronic disease, the area in which they can serve humanity the most. use. I am deeply grateful to each of you for helping to create this incredible opportunity to change medicine for the better.
Author’s Note: This is an abridged version of a more in-depth article that shares the most effective strategies we have found to ensure that the hospital is providing you or your loved ones with optimal medical care, and discusses other approaches we have found can significantly improve patient survival (e.g., adequate intravenous hydration to restore physiologic zeta potential). You can read that article and its other links here.
Note from Dr. Mercola to the Author
A Midwestern Physician (AMD) is a board-certified Midwestern physician and longtime reader of Mercola.com. I appreciate AMD’s exceptional insights on a variety of topics and am grateful to be able to share them. I also respect AMD’s wish to remain anonymous, as AMD is still at the forefront of treating patients. For more of AMD’s work, check out The Forgotten Side of Medicine on Substack.
Sources:
- 1 FLCCC Alliance, November 9, 2021
- 2 Amazon, War on Ivermectin: The Medicine that Saved Millions and Could Have Ended the Pandemic
- 3 Health System Tracker, December 15, 2023
- 4 US Government Spending, Health Care Spending
- 5, 6 The Commonwealth Fund, January 31, 2023
- 7 The OECD Data Explorer
- 8 Wikipedia, Joint Commission
- 9 Health Serv Res. 2004 Jun;39(3):627–642
- 10, 11 Health Serv Res. 2002 Dec;37(6):1625–1642
- 12 Debt.org, November 30, 2023
- 13, 16 Am j Hosp Med 2021 Dec;5(4):2021
- 14 The Joint Commission, Critical Access Hospital Accreditation Fact Sheet
- 15 CMS.gov, September 10, 2024
- 17 Ann Surg Oncol. 2021 Jan 3;28(3):1263–1264
- 18 NIH National Institute of General Medical Sciences, July 2024
- 19 Repurposed Drugs: Powers & Possibilities, January 14, 2024
- 20 Chest. 2017 Jun;151(6):1229-1238
- 21 Cleveland Clinic, April 19, 2022
- 22 JAMA Netw Open. 2024;7(7):e2424984
Source: https://articles.mercola.com/sites/articles/archive/2024/12/13/hospitalization.aspx
Image: Pixabay.com